Improve your POP now!
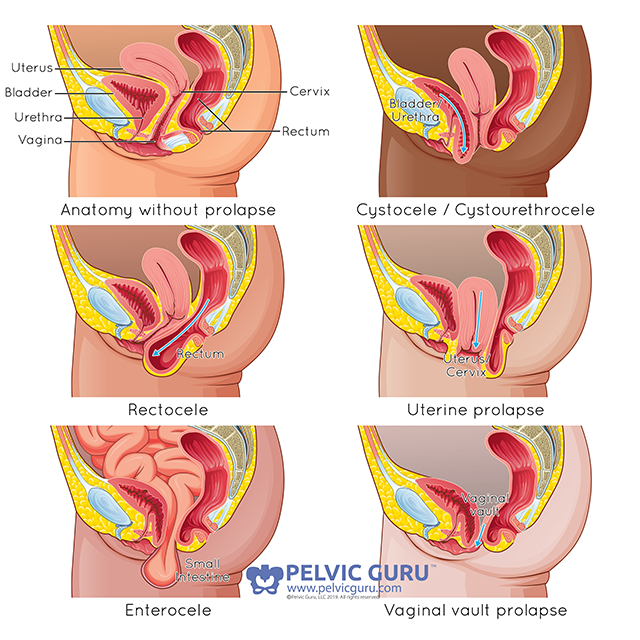
Types of Pelvic Organ Prolapse
Permission to use copyright image from Pelvic Guru, LLC pelvicguru.com
A diagnosis of pelvic organ prolapse (POP) can bring on stressful feelings of disappointment, fear, insecurity & uncertainty
I hope when you were told about your POP, it was followed up with options & optimism. Not just “when your done having kids we can talk about surgery” 🙉
I also hope you were told how common POP is among postpartum women. It is so common, that in fact, a grade 1 prolapse is almost considered the postpartum “norm”. Prevalence ranges up to 85%!! Many women have prolapse but have no symptoms. Symptoms do not necessarily coincide with the grade of prolapse either. This is why it is so important to be checked & ask questions! Although vaginal delivery is a big risk factor, women who birthed via cesarean, those who have never had a baby & even men can still develop prolapse. It is a result of weak tissues, hormone fluctuation and poor pressure management.
Why wait until then to “fix” your POP, when you can start now, improve it/prevent it from becoming worse, & hopefully avoid the need for surgical intervention down the road?
Some options you can start TODAY include:
Pelvic Floor Strengthening- Our pelvic floor acts as a hammock to help support our internal organs. When we are dealing with prolapse, there is laxity in the tissues. Have a supportive pelvic floor will help further support & suspend these tissues.
Try to avoid adding increased pressure in your abdomen & on the pelvic floor. As women, we almost get accustomed to sucking in our belly/gut which also leads to a shallow breathing pattern and tends to make us hold our breath. A lot of women have done this for so long they don’t even notice they are doing it! Sometimes even tight fitting clothes may do this & can make your symptoms worse.
Try different postures. Ideally I like to preach ribs stacked over hips but every body is different & everyone’s symptoms respond differently. Look at yourself sideways in a mirror and see if your resting posture is shoulders behind hips or vice versa & give the stacked posture a try to see how your symptoms react. Some people even benefit from a little tilt in their pelvis either anterior (fwd, like sticking your butt out) or posterior (bwd, like tucking your tail).
Pay attention to what exercises or activities make your symptoms worse and try to scale back so you can control those symptoms. For example, if your typical exercise is running but the impact on the pavement doesn’t feel good on the PF, try trail running or on a treadmill for less impact. I have pts that have turned to cycling on days when their symptoms are bad because the support from the saddle really helps with their symptoms. If any exercises or activities in your normal routine bring on your symptoms, this may mean these activities are a little too advanced for what your system can manage at this time. We spend a lot of time in PT finding the right intensity or level of exercise for you and then advance you as your system gets more efficient. You will get back to your normal routine, but you have to meet your body where your PF is ☺️
Speaking of support- look into external supports. These can be extremely helpful and feel pretty good for patients with POP. My most recommended are the V-2 & PF Press from @itsyoubabe and the postpartum bloomers from @baobeimaternity. I also highly recommend them for everyone in the initial postpartum phase as everyone could use a little extra support down there as their body heals.
Regulate your bowels🚽. Constipation once again causes increased pressure. Straining to have a BM causes even more. Drink lots of water, ⬆️ your fiber intake & exercise regularly (more detailed post on this coming soon!)